The interpretation of thyroid function tests is a very popular exam topic. Thyroid disease is common, affecting approximately 1% of the female population, and there is a wide range of conditions affecting the thyroid gland, with a wide range of clinical features. For this reason, thyroid function tests (TFTs) are amongst the most commonly requested laboratory investigations in both the primary and secondary care settings.
Basic thyroid physiology
In order to accurately interpret the results of thyroid function tests, a basic understanding of the physiology of the thyroid is required.
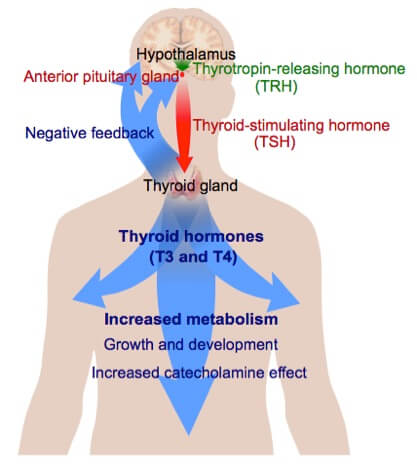
The thyroid gland produces the thyroid hormones thyroxine (T4) and tri-iodothyronine (T3), as well as the peptide hormone calcitonin. The thyroid hormones are responsible for a wide range of processes, including control of the basal metabolic rate, cellular respiration, total energy expenditure, growth and development, and cardiovascular effects.
The release of the T3 and T4 into the bloodstream is controlled by a negative feedback system involving the hypothalamic-pituitary-thyroid axis. A low metabolic rate or a decrease in serum T3 and/or T4 levels causes the secretion of thyrotropin-releasing hormone (TRH) from the hypothalamus. TRH then travels to the anterior pituitary gland and stimulates secretion of thyroid-stimulating hormone (TSH). Conversely, elevated serum levels of thyroid hormones inhibit the release of TRH and TSH.
Following its release by the pituitary gland, TSH stimulates the thyroid gland to manufacture and release stored T3 and T4 until the metabolic rate is normalised. Thyroperoxidase is synthesised within the endoplasmic reticulum of the thyrocyte and oxidises iodine, which is a critical component of the thyroid hormones. This subsequently results in the formation of T3 and T4. T3 is the active hormone and has roughly three times the metabolic potency of T4, and T4 is the prohormone, which is broken down in the tissues to form T3 when required.
T3 and T4 are over 95% protein bound, and this is predominantly to thyroid binding globulin (TBG). TBG levels are generally unaltered in primary hypothyroidism and thyrotoxicosis, and conditions that alter TBG levels tend to change total T3 and T4 levels but not free T3 and T4 levels.
Reference ranges
Different testing laboratories tend to have slightly different reference ranges, but the normal ranges for thyroid function tests as per the British Thyroid Foundation are:
| Test | From | To | Units |
|---|---|---|---|
| TSH | 0.4 | 4.0 | mU/L |
| Free T4 | 9.0 | 25.0 | pmol/L |
| Free T3 | 3.5 | 7.8 | pmol/L |
Hypothyroidism
A high TSH level with a low Free T4 (FT4) level indicates hypothyroidism.
Hypothyroidism generally develops slowly over a period of months or years. Often in the early stages of the disease, free T3 and T4 levels are normal, and the earliest biochemical change that is noticed is generally a rise in thyroid stimulating hormone (TSH) levels.
If the TSH is low or normal and FT4 is normal, then thyroid status is also considered to be normal. If the TSH is elevated, but the FT4 is normal, then subclinical hypothyroidism exists. Generally speaking, thyroxine replacement therapy is considered if the TSH is > 12 mU/L. If the TSH is mildly elevated (in the range of 4-12 mU/L), and thyroperoxidase antibodies are positive, then this indicates a future risk of developing hypothyroidism of approximately 5% per year.
Hyperthyroidism
A low TSH level with a high FT4 level and a high FT3 level indicates hyperthyroidism. TSH is the most helpful test when screening for thyroid dysfunction in non-critically ill patients, as TSH is almost always suppressed in hyperthyroidism. A raised FT4 and FT3 with suppressed TSH and an elevated TSH receptor antibody level confirms a diagnosis of Grave’s disease.
A small number of cases will have a normal FT4 level with a suppressed TSH level. In these cases, a FT3 level should be measured, as it is likely to be a diagnosis of T3 thyrotoxicosis.
Sick euthyroid syndrome
Sick euthyroid syndrome is a condition in which there is dysregulation of the hypothalamic-pituitary-thyroid axis, causing a reduction of FT4 level and/or FT3 levels in a clinically euthyroid patient with a non-thyroidal systemic illness. It is most commonly seen in starvation, critical illness, or the intensive care setting. TSH levels are usually low or normal in sick euthyroid syndrome.Thyroid function test results usually return to normal when the patient is restored to good health.
Drug therapies that interfere with thyroid function testing
The following table outlines the effects of the drugs that most commonly interfere with thyroid function tests:
| Drug Therapy | Effects on TFTs |
| Amiodarone | Interferes with synthesis of TSH Interferes with peripheral conversion of T4 to T3 Inhibits entry of T4 and T3 into peripheral tissues >50% of patients on long-term amiodarone have abnormal TFTs Most commonly causes suppression but can cause hypo- or hyperthyroidism |
| Lithium | Interferes with both the synthesis of thyroid hormones and their release from the gland Long-term lithium treatment causes goitre in approx. 50% of patients Subclinical hypothyroidism occurs in approx. 20% |
| Beta-blockers | Interferes with the conversion of T4 to T3 Generally doesn't cause clinical hypothyroidism but can affect TFTs |
| Corticosteroids | Transiently suppresses TSH secretion for a few hours after administration Patients taking corticosteroids should have TFTs measured prior to administration of morning dose |
| NSAIDs and high-dose aspirin | Can cause analytical interference resulting in inaccurate TFT results |
Monitoring thyroxine replacement therapy
In patients with primary hypothyroidism taking thyroxine replacement therapy, the adequacy of treatment is generally monitored via a combination of TSH levels and clinical symptoms.TSH levels take around 4-6 weeks to stabilise, and for this reason, it is recommended that this period is left before re-checking TFTs following initiation of therapy or dose alteration.
FT4 levels can be used to assess recent patient compliance. Patients who are usually non-compliant but start taking their thyroxine a few days before their blood tests typically have a normal or raised FT4 with a paradoxically elevated TSH.
TSH results in compliant patients can be interpreted as follows:
- < 0.05 mU/L – over replacement
- 05-0.2 mU/L – possible over replacement
- 2-2.0 mU/L – optimal replacement
- >0mU/L – likely under replacement
Thank you to the joint editorial team of MRCGP Exam Prep for this exam tips post.
Header image used on licence from Shutterstock