Pregnancy, which is also referred to as gestation, is the period during which one or more offspring develop inside a woman.
Definitions
Pregnancy is divided into three stages, each of which is marked by specific foetal developments:
- First trimester: 0 to 12 weeks
- Second trimester: 12 to 28 weeks
- Third trimester: 28 weeks to delivery
A pre-term delivery occurs when the baby is born alive before 37 weeks of gestation are completed. This usually refers to the period between 24 and 37 weeks.
A post-term delivery occurs when the baby is born after 42 weeks of gestation.
The gestational age is the term used to describe how far along the pregnancy is. It is measured in weeks, from the first day of the mother’s last menstrual period (LMP) to the current date.
The estimated date of delivery (EDD) is calculated using Naegele’s rule. It is calculated by starting on the first day of the LMP, adding one year, subtracting 3 months, and then adding 7 days:
EDD = LMP + 1 year – 3 months + 7 days
Blastocyst formation
Following fertilisation, the zygote cleaves into two blastomeres. The cleavage process continues for an additional 3 days until a compact mass called the morula is produced. The morula is an early-stage embryo, consisting of 16 blastomere cells, in a sold ball contained within the zona pellucida.
The morula then enters the uterine cavity, where cell division continues, and fluid accumulates between the cells of the morula. This produces the early blastocyst on the fourth day following fertilisation. The early blastocyst comprises an inner cell mass (5 cells that will give rise to the embryo) and trophectoderm (53 cells that will give rise to trophoblast).
After two days of free-floating in the uterine fluid, the secretory-phase endometrial glands produce proteases that liberate the blastocyst from the zona pellucida. This process is referred to as embryo hatching. Hormones and cytokines produced by the blastocyst now directly influence the endometrium and promote receptivity. At this stage, the embryo starts to absorb nutrients from the uterine secretions.
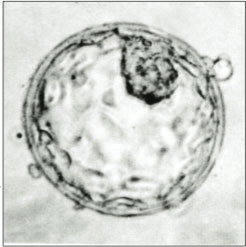
A human blastocyst, with the inner cell mass visible upper right
Implantation
The process of implantation process is mediated by receptors on the blastocyst and endometrium and by oestrogen and progesterone release from the corpus luteum. For this reason, the uterus is only receptive to implantation between days 20 and 24 of the menstrual cycle.
Implantation is most likely to occur around 6 to 7 days after fertilisation. This happens in three phases:
- Phase 1 (Apposition) – the blastocyst is apposed, in most cases, to the upper posterior uterine wall
- Phase 2 (Adhesion) – there is increased physical contact between the blastocyst and the uterine wall
- Phase 3 (Invasion) – the blastocyst penetrates the endometrium, the upper third of myometrium, and the uterine vasculature. By day 10, the blastocyst is completely encased in endometrium.
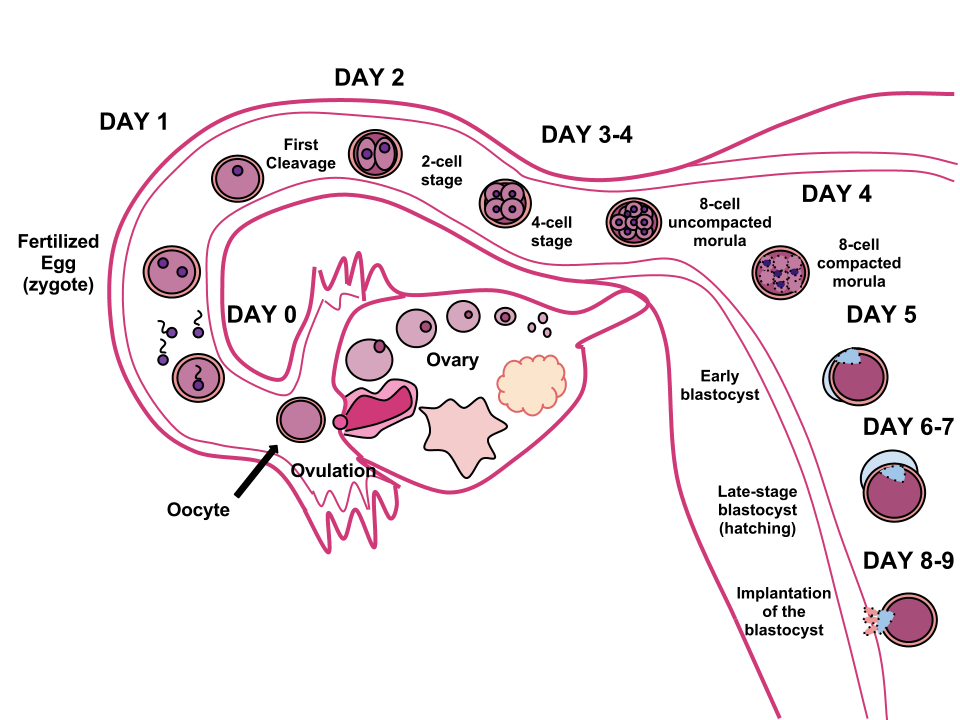
The process of fertilisation and implantation, image sourced from Wikipedia
Courtesy of Ttrue12 CC BY-SA 3.0
Trophoblast differentiation
Troophoblasts are cells that are derived from the trophectoderm cells on the outer layer of the blastocyst. By day 8 following fertilisation, these trophoblast cells have differentiated into two cell layers, the cytotrophoblast and the syncytiotrophoblast.
The cytotrophoblast is the single-celled inner layer of the trophoblast, and the syncytiotrophoblast is the multinucleated syncytium that makes up the outer layer. The syncytiotrophoblast lacks cell boundaries and grows into the endometrial stroma. It secretes hCG in order to maintain progesterone secretion and sustain the pregnancy.
Trophoblast cells further differentiate into villous and extravillous trophoblast. Villous trophoblast cells give rise to chorionic villi and are responsible for oxygen and nutrient transport between mother and foetus. Extravillous trophoblast cells migrate deeper into the uterine wall and penetrate the maternal vasculature (endovascular extravillous cells invade the uterine spiral arteries, while interstitial extravillous cells surround the spiral arteries). As the trophoblast cells are differentiating and invading the endometrium, the inner cell mass differentiates into ectoderm and endoderm.
The yolk sac
The yolk sac is the first element seen in the gestational sac during pregnancy, at approximately 3 days gestation. The yolk sac is situated on the ventral aspect of the embryo. It is lined by extra-embryonic endoderm. The yolk sac plays no part in supporting the nutrition of the developing human embryo, which is a role solely carried out by the placenta.
Blood is conveyed to the wall of the yolk sac by the primitive aorta, and after circulating through a wide-meshed capillary plexus, is returned by the vitelline veins to the tubular heart of the embryo. This constitutes the vitelline circulation, which is the initial site of haematopoiesis.
At the end of the fourth week, the yolk sac presents the appearance of a small pear-shaped opening (traditionally called the umbilical vesicle) into the digestive tube by a long narrow tube, the vitelline duct. The dorsal part of the yolk sac is incorporated into the embryo, forming the gut.
A hollow fluid-filled, sac-like structure called the allantois projects from the yolk sac and later, the hindgut. The allantois forms an axis for the development of the umbilical cord. It becomes surrounded by the mesodermal connecting stalk, called the body stalk. The vasculature of the body stalk develops into the umbilical arteries that carry deoxygenated blood to the placenta.
The decidua
The decidua is the modified mucosal lining of the uterus (modified endometrium) that forms in preparation for pregnancy by a process called decidualisation. It is formed under the influence of progesterone, which stimulates endometrial stromal cells to swell and store nutrients. The decidua is the only source of nutrients for the embryo in the first week after implantation.
The part of the decidua that interacts with the trophoblast is the decidua basalis (also called the decidua placentalis), while the decidua capsularis grows over the embryo on the luminal side, enclosing it into the endometrium. The remainder of the decidua is termed the decidua parietalis or decidua vera, and it will fuse with the decidua capsularis by the fourth month of gestation.
There are three morphologically distinct layers of the decidua basalis:
- Compact outer layer (stratum compactum)
- Intermediate layer (stratum spongiosum)
- Boundary layer adjacent to the myometrium (stratum basalis)
The amnion and amniotic fluid
The amnion is a membrane that closely covers the embryo when it is first formed. Over time, it fills with amniotic fluid, which causes the amnion to expand and become the amniotic sac, providing a protective environment for the developing embryo.
In the earliest stages of embryonic development, the amnion appears as a closed sac in the inner cell mass as a cavity. This cavity is roofed by a single layer of ectodermal cells called the amniotic ectoderm. This layer gives rise to amnion epithelial cells, which form the amnion.
The amnion is initially located on the dorsal surface of the embryo but eventually covers it entirely. As the amnion grows, it obliterates the yolk sac and covers the body stalk. It eventually fills the intra-uterine space, and the body stalk is unsheathed by the amnion and becomes the umbilical cord.
The amnion provides most of the tensile strength of the membranes. It lacks smooth muscle cells, nerves, lymphatics, and blood vessels but is responsible for amniotic fluid homeostasis through salt and water transport. Initially, the amniotic fluid consists of an ultrafiltrate of maternal plasma, but as the foetus grows, fluid diffuses through its skin and begins to influence the makeup of amniotic fluid.
By week 12, the foetal kidneys begin to produce urine, which further contributes to the amniotic fluid. The amniotic fluid serves to cushion the foetus, allowing movement and musculoskeletal development and minimising the risk of trauma.
The chorion and chorionic villi
The chorion is the outermost foetal membrane around the embryo. It develops from an outer fold on the surface of the yolk sac called the vitelline membrane. It undergoes rapid proliferation and forms numerous processes, called the chorionic villi, that invade and obliterate the uterine decidua. These chorionic villi serve to maximise the available contact area with maternal blood.
The chorionic villi undergo several stages, depending on their composition. These are summarised in the table below:
| Stage | Period of gestation | Description |
|---|---|---|
| Primary villi | 13-15 days | These are solid outgrowths of cytotrophoblasts that protrude into the syncytiotrophoblasts. These are initially small and non-vascular. |
| Secondary villi | 16-21 days | The primary villi are invaded by embryonic mesenchymal cells to form the secondary villi. The villi increase in size and ramify while the mesoderm grows into them. The cytotrophoblast cells become less prominent, and the connective tissue stroma is more densely packed in order to minimise the distance across the villi. |
| Tertiary villi | 17-22 days | The mesenchymal cells undergo angiogenesis, producing chorionic vessels to receive nutrients from the maternal circulation, resulting in tertiary villi. Branches of the umbilical artery and umbilical vein grow into the mesoderm and connect with the chorionic vessels via the umbilical cord, forming the foetal-placental circulation. In addition to the tertiary villi, there are also anchoring villi, which are extensions of syncytiotrophoblasts and cytotrophoblasts that connect the chorionic plate to the decidual basal plate (the roof of the intervillous space). |
The embryonic period
The embryonic period begins 2-3 weeks after ovulation and lasts 8 weeks; organogenesis occurs during this period. At the beginning of the embryonic period, the embryonic disc is well-defined, the body stalk is differentiated, and a true intervillous space exists.
In week 3, foetal blood vessels develop in the chorionic villi. In week 4, the true maternal-foetal circulation and a rudimentary foetal cardiovascular system are established. Partitioning of the heart commences at this stage. By the end of week 6, the heart is completely formed, fingers and toes are present, and the ears are present as elevations on the head.
The foetal period
The foetal period commences 10 weeks after the LMP and lasts until birth.
Growth and maturation of the organs formed in the embryonic period occur in this stage.
During weeks 10 to 12, the foetus starts to swallow can swallow, the small intestine starts to undergo peristalsis and glucose transport begins. In week 12, the ossification centres appear in bones, the genitalia begin to differentiate, and skin, nails and hair appear.
During weeks 20 to 24, neuronal migration and proliferation are completed, and neurologic development shifts towards increasing neuronal organisation and differentiation. By week 24, the bronchioles and alveoli are nearly completely developed, but terminal alveolar sacs are typically not yet formed. The foetus will, therefore, be unlikely to be able unable to breathe at this stage.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this article.