Arterial blood gas (ABG) interpretation helps us with the assessment of a patient’s respiratory gas exchange and acid-base balance. It forms a key part of the management of sick patients and provides invaluable information, particularly when combined with a thorough clinical assessment.
Normal arterial blood gas values
The normal values on an ABG can vary a little between analysers, but broadly speaking are as follows:
| Variable | Range |
|---|---|
| pH | 7.35 – 7.45 |
| PaO2 | 10 – 14 kPa |
| PaCO2 | 4.5 – 6 kPa |
| HCO3- | 22 – 26 mmol/l |
| Base excess | -2 – 2 mmol/l |
In order to properly interpret an ABG an understanding of each of the key components of an arterial blood gas is necessary.
pH
The pH of a solution is a figure expressing the acidity or alkalinity of a solution on a logarithmic scale on which 7 is neutral, lower values are acidic, and higher values are alkaline. The scale is inversely proportional to the concentration of hydrogen ions in the solution.
The body’s pH is maintained within a range of 7.35 to 7.45 under normal circumstances and this homeostasis is achieved through the buffering and excretion of acids. Important buffers include plasma proteins and bicarbonate extracellularly, and proteins, phosphate, and haemoglobin intracellularly.
This buffering system provides only a temporary solution to the production of acids, and once the buffers are consumed acids will begin to accumulate. A system of acid excretion therefore exists, which allows time for the regeneration of buffers. This system occurs via the kidneys and the lungs, with hydrogen ions being excreted via the kidney and carbon dioxide being excreted via the lungs.
If both the buffering and renal excretion systems are overwhelmed then the pH will fall and a metabolic acidosis will occur. If the ability of the lungs to excrete carbon dioxide is compromised then a respiratory acidosis will occur.
Partial pressure (PP)
Partial pressure is the pressure that would be exerted by one of the gases in a mixture if it occupied the same volume on its own. For example, air at sea level has an approximate pressure of 100 kPa, oxygen composes 21% of this, and therefore oxygen has a partial pressure of 21 kPa at sea level. If the total pressure of the mixture is doubled, in this case to 200 kPa, the percentage of oxygen within the mixture will remain 21%, but the partial pressure of oxygen will now be 42 kPa.
Henry’s law states that: “At a constant temperature, the amount of a given gas in a given type and volume of liquid is directly proportional to the partial pressure of that gas in equilibrium with that liquid.” Therefore it can be seen that bearing this law in mind, arterial blood gases can be used to measure the pressure of gases in the blood:
- PaO2 – is the partial pressure of oxygen in arterial blood (10-14 kPa)
- PaCO2 – is the partial pressure of carbon dioxide in arterial blood (4.5-6 kPa)
Bicarbonate (HCO3-)
Bicarbonate is the most important buffer and is produced by the kidneys. It is a base, which is the opposite of an acid. The normal range for bicarbonate is 22 – 26 mmol/l.
In the presence of excess acid within the blood, bicarbonate will neutralize the hydrogen ions via the following reaction, preventing an increase in plasma pH:
[H+] + [HCO3-] ⇌ [ H2CO3]
In the presence of a chronic acidosis the kidneys produce additional bicarbonate to maintain the pH within the normal range.
Base excess (BE)
The base excess is a measure of the amount of excess acid or base present in the blood as a consequence of metabolic derangement. It is calculated as the amount of strong base that would need to be added or subtracted from a substance in order to return it to a normal pH of 7.40. The normal range for base excess is -2 – 2 mmol/l.
Any value that lies outside of this normal range of suggestive of a metabolic cause for the acidosis or alkalosis:
- A BE of less than -2 mmol/l is suggestive of a metabolic acidosis
- A BE of more than +2 mmol/l is suggestive of a metabolic alkalosis
Other components of the arterial blood gas
There is considerable variation between different analysers, but any or all of the following values may also be present:
- Electrolytes
- Glucose
- Lactate
- Haemoglobin
- Carbon monoxide
- Methaemoglobin
Compensation
As we have already learned, the pH of the human body is tightly maintained within a range of 7.35 – 7.45 via respiratory and metabolic compensatory mechanisms.
Respiratory compensation occurs in response to metabolic acidosis. The change in pH is detected by central chemoreceptors in the medulla, and peripheral chemoreceptors in the carotid bodies. This results in an increase in the rate and depth of respiration, which in turn increases CO2 excretion in an attempt to normalise the pH.
Metabolic compensation occurs in response to respiratory acidosis, for example CO2 retention in chronic lung disease. In these circumstances bicarbonate is retained by the kidneys in an attempt to normalise the pH. Unlike respiratory compensation, this process occurs slowly over a period of a few days.
Respiratory failure
Respiratory failure occurs when the respiratory system fails in either one or both of its gas exchange functions: oxygenation and the elimination of carbon dioxide. A reduction in the oxygen carried in the bloodstream is referred to as hypoxaemia, and a rise in the carbon dioxide levels within the bloodstream is referred to as hypercapnia.
Respiratory failure is classified into two groups:
- Type I respiratory failure
- Type II respiratory failure
Type I respiratory failure occurs when there is a problem with oxygenation resulting in hypoxaemia. This is most commonly caused by ventilation/perfusion mismatch resulting in reduced diffusion of oxygen from the alveoli into the pulmonary circulation. Type I respiratory failure is characterized by:
- Reduced PaO2 (<8.0 kPa or 60 mmHg)
- Normal or reduced PaCO2 (<6.7 kPa or 50 mmHg)
Type II respiratory failure occurs when there occurs when there is inadequate alveolar ventilation resulting in hypoxaemia and hypercapnia. Type II respiratory failure is characterized by:
- Reduced PaO2 (<8.0 kPa or 60 mmHg)
- Elevated PaCO2 (>6.7 kPa or 50 mmHg)
- Reduced pH (<7.35)
Type II respiratory failure can be further sub-classified depending on the pre-existing condition of the patient and the speed of onset:
- Acute type II respiratory failure: the patient will have no, or minor, evidence of pre-existing respiratory disease and patients typically have a high PaCO2, low pH, and normal bicarbonate
- Chronic type II respiratory failure: evidence of chronic respiratory disease, high PaCO2, normal pH, and high bicarbonate (>26 mmol/l).
Acute-on-chronic type II respiratory failure: an acute deterioration in an individual with significant pre-existing type II respiratory failure, high PaCO2, low pH, and high bicarbonate (>26 mmol/l).
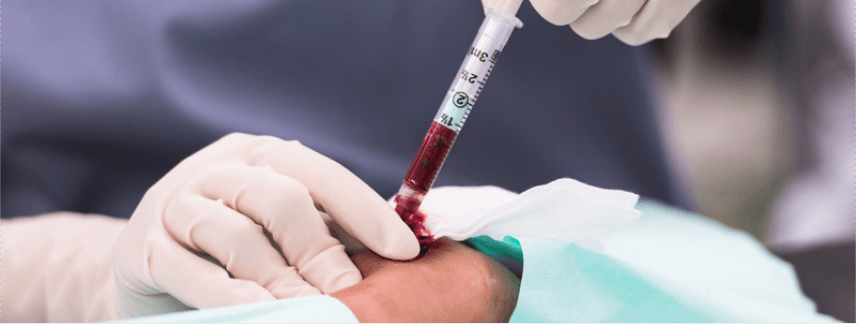
Header image used on licence from Shutterstock
Next: Arterial Blood Gas Analysis Part 2 – Interpreting the Results
Thank you to the joint editorial team of www.mrcemexamprep.net for this article.






…a very help ful basic knowledge.
Very very informative
Thanks
I always love to read every stuff that you send me to improve my knowledge. Thanks for great work as ever.
Explained a very informative and organised way about the basic knowledge of ABG and its interpretation.
very nice information…
thanks