Globally, approximately 50 million people have dementia, and there are nearly 10 million new cases every year.
Dementia is a syndrome in which there is deterioration in memory, thinking, behaviour and the ability to perform everyday activities. Although dementia mainly affects older people, it is not a normal part of ageing. In rarer cases, it can also affect younger people.
There are several different causes of dementia, all of which have overlapping features, which can cause confusion when making a diagnosis. For this reason, they are a common topic in medical exams. In this exam tips article, we will look at some of the more commonly tested one and highlight the features that will help you to ascertain the most likely diagnosis.
Alzheimer’s disease
Alzheimer’s disease is the most common cause of dementia, accounting for around 50% of all cases. It involves progressive degeneration of the cerebral cortex, with cortical atrophy, neurofibrillary tangles, amyloid plaque formation and reduction in acetylcholine production from affected neurons. The cause is not yet fully understood.
The onset of Alzheimer’s disease is typically gradual and insidious. It progresses slowly over 7-10 years with different symptoms being present depending on the stage of the disease.
In the early stages of Alzheimer’s disease, the patient is frequently noticed to be forgetful by relatives and friends, with lapses in memory evident. Forgetting the names of people and places and having difficulty finding words for things is commonly seen. The patient also often cannot remember recent events and forgets appointments. As the disease progresses, difficulty with language skills and problems with planning and decision making develop. Apraxia can occur, and the patient is noticed to be more obviously confused.
In the later stages, symptoms include wandering, disorientation and apathy. Psychiatric symptoms also develop in this stage, with depression being common. Psychotic symptoms, such as hallucinations and delusions, may also be seen. Late in the disease, there may also be behavioural problems, such as disinhibition, aggression, agitation, and this can be very distressing for the family.
Vascular dementia
Vascular dementia is the second leading cause of dementia, accounting for around 25% of all cases. It involves damage to the brain caused by a variety of different mechanisms, including major strokes, multiple smaller unrecognised strokes (multi-infarct) or chronic changes in smaller vessels (subcortical dementia). Increasingly the term vascular cognitive impairment (VCI) is used to encompass this spectrum of disease.
In contrast to Alzheimer’s disease, which is characterised by a slow and insidious onset, vascular dementia can occur suddenly and typically has a series of stepwise increases in symptom severity. The presentation can vary significantly, though, as can the speed of progression.
Features that are more suggestive of a vascular cause of dementia include:
- History of TIAs or cardiovascular disease
- Presence of focal neurological abnormalities
- Prominent memory impairment in the early stages of disease
- Early presence of disturbance in gait and unsteadiness
- Frequent, unprovoked falls in early stages
- Bladder symptoms (e.g. incontinence) without a demonstrable urological condition in early stages
- Seizures
Dementia with Lewy bodies (DLB)
Dementia with Lewy bodies (DLB), which is also referred to as Lewy body dementia (LBD), is a progressive neurodegenerative dementia that is closely associated with Parkinson’s disease (PD). It is the third most common cause of dementia in the elderly after Alzheimer’s disease and vascular dementia, accounting for approximately 15% of cases.
The clinical features of DLB include:
- Mild features of Parkinsonism or co-existing PD
- Progressive decline in cognitive function
- Fluctuations in cognition, alertness and attention span
- Episodes of transient loss of consciousness
- Recurrent falls
- Visual hallucinations
- Depression
- Complex, systematized delusions
The level of cognitive impairment often fluctuates from hour-to-hour and from day-to-day.
Pathologically DLB is characterized by the development of abnormal collections of protein within the cytoplasm of neurons (Lewy bodies). These intracellular protein collections have similar structural features to the ‘classical’ Lewy bodies seen in Parkinson’s disease:
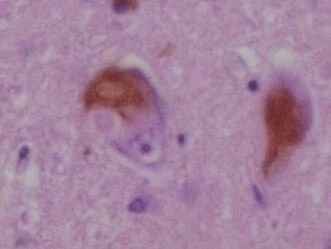
Courtesy of Dr. Andreas Becker CC BY-SA 3.0
Frontotemporal dementia
Frontotemporal dementia (FTD) is a progressive neurodegenerative condition that primarily affects the frontal and/or temporal lobes of the brain. It is now recognised as part of a broader group of overlapping syndromes, which are more common than previously believed.
One subtype of FTD is Pick’s disease (PiD). However, the terms Pick’s disease and frontotemporal dementia should not be used interchangeably, as PiD represents only a specific form within the wider spectrum of frontotemporal dementia syndromes.
Pick’s disease is a rare neurodegenerative disorder that causes a slowly progressive frontotemporal dementia. A defining characteristic of the disorder is the build-up of tau proteins in neurons, accumulating into silver-staining, spherical aggregations referred to as ‘Pick bodies’.
Pick’s disease is a rare neurodegenerative condition that leads to a slowly progressive form of frontotemporal dementia. It is characterised by the accumulation of tau proteins within neurons, forming distinctive silver-staining, spherical structures known as Pick bodies.
The usual age of onset is between 40 and 60 years of age. It is initially characterized by personality changes such as:
- Disinhibition, tactlessness and vulgarity
- Changes in moral values
- Efforts to dissociate from family
- Problems with concentration
- Over-activity, pacing and wandering
The changes in personality occurring before memory loss allow Pick’s disease to be distinguished from Alzheimer’s disease. As the disease progresses the patient will develop deficits in intellect, memory and language.
Huntingdon’s disease
Huntington’s disease (HD) is an autosomal dominant, progressive neurodegenerative disorder marked by a characteristic combination of chorea, dystonia, incoordination, cognitive decline, and behavioural disturbances.
It is caused by an expanded cysteine-adenosine-guanine (CAG) triplet repeat within the huntingtin (HTT) gene located on chromosome 4p16.3. Expression of the mutated gene leads to widespread cellular changes, particularly cell loss in the basal ganglia and cerebral cortex.
HD typically presents between the ages of 30 and 50 but can develop at any age. A prodromal phase often precedes the onset of chorea, featuring mild psychotic symptoms and behavioural changes.
Early signs include personality shifts, self-neglect, apathy, clumsiness, fidgeting, and fleeting facial grimaces. Behavioural problems are common and may lead to family conflict, marital breakdown, or job loss even before a formal diagnosis is made.
As the disease progresses, it causes worsening chorea, rigidity, and dementia. Seizures are also relatively common. Chorea starts mildly but can become severe, leading to uncontrollable limb movements.
Over time, dystonia and Parkinsonian features gradually replace the chorea. Dysarthria, dysphagia, and abnormal eye movements are frequent complications in advanced stages.
Pseudodementia
Pseudodementia, also sometimes referred to as depression-related cognitive dysfunction, is a condition in which there is a temporary decline in cognitive function in combination with a functional psychiatric condition.
Depression is most commonly the cause, but it is seen in a wide range of psychiatric conditions including schizophrenia, bipolar disorder and hysteria. It is reversible with treatment of the underlying psychiatric condition. It is associated with a relatively high-risk of suicide.
Features that are consistent with a diagnosis of pseudodementia include:
- History of a psychiatric condition
- Sudden onset
- Presence of insight
- A tendency to emphasise disability
- Absence of changes in cognition at night
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcgpexamprep.co.uk for this ‘Exam Tips’ post.