The initial assessment of the patient with thermal injuries involves the following steps. There are multiple priorities in a burned patient, and in reality, these are usually managed in parallel or a horizontal manner by a fully trained resuscitation team:
- Stop the burning process
- Establish airway control
- Ensure adequate ventilation
- Manage circulation with burn shock resuscitation.
Stop the burning process
It is of the utmost importance to completely remove the patient’s clothing to stop the burning process. Any clothing that us adherent to the patient should not be peeled, but instead should be cut around, actively cooled and left for formal debridement.
Any debris or contaminants that are present in the burn should be removed by rinsing with copious amounts of warm saline irrigation. After the burning process has been stopped, the patient should be covered and kept warm to prevent hypothermia.
Establish Airway Control
Early evaluation of the airway is a crucial part of the management of a burned patient. Airway obstruction can occur rapidly, both as a consequence of direct injury (e.g. inhalation injury), and also from oedema resulting from the burn injury. If there is an associated history of trauma, the airway should be assessed and managed with cervical spine control in place.
Signs of airway obstruction can be subtle at the time of presentation as oedema is typically not present initially. Children with thermal burns are at higher risk for airway obstruction than adults because of the relatively smaller airway size, and they should be observed very carefully.
Risk factors for airway obstruction in a burned patient include the following:
- Inhalation injury
- Soot in the mouth or nostrils
- Singed nasal hairs
- Burns to head, face and neck
- Burns inside the mouth
- Large burn area and increasing burn depth
- Associated trauma
- A carboxyhaemoglobin level >10% (suggestive of an inhalation injury).
Definitive airway management with an uncut endotracheal tube may be needed urgently before significant oedema develops. If there is a delay in recognition of impending airway obstruction, airway oedema can impede intubation, and a surgical airway may be required.
The American Burn Life Support (ABLS) indications for early intubation include:
- Signs of airway obstruction (hoarseness, stridor, accessory respiratory muscle use, sternal retraction)
- Extent of the burn (total body surface area burn > 40%–50%)
- Extensive and deep facial burns
- Burns inside the mouth
- Significant oedema or risk for oedema
- Difficulty swallowing
- Signs of respiratory compromise: inability to clear secretions, respiratory fatigue, poor oxygenation or ventilation
- Decreased level of consciousness where airway protective reflexes are impaired
- Anticipated patient transfer of large burn with airway issue without qualified personnel to intubate en route.
Circumferential burns of the neck can lead to swelling of the tissues around the airway; therefore, early intubation is also indicated for full-thickness circumferential neck burns.
Ensure adequate ventilation
Patients with burns should usually be administered high-flow (15 L) oxygen via a reservoir bag while their breathing is being assessed. If intubation is necessary, it is vital to use an appropriately sized endotracheal tube (ETT). A tube that is too small will make ventilation, clearing of secretions, and bronchoscopy difficult or impossible. ETTs at least size 7.5 mm internal diameter (ID) or larger in adults, and at least size 4.5 mm ID ETT in children are recommended. In those patients that have been intubated, 100% oxygen should be continued until carboxyhaemoglobin levels fall to <5%. Lung protective ventilation should be used with low tidal volumes (4-8 mL/kg) and peak inspiratory pressures <30 cmH2O.
If the patient’s hemodynamic condition permits and spinal cord injury has been excluded, then the patient’s head and chest should be elevated by approximately 30 degrees to help reduce chest wall and neck oedema. Circumferential full-thickness burns of the chest wall will require emergency escharotomy. Full-thickness burns of the anterior and lateral chest wall may also result in a significant restriction of chest wall motion that necessitate escharotomy.
Breathing problems in a burned patient tend to arise as a result of one of or a combination of the following three causes:
- Hypoxia
- Smoke inhalation
- Carbon monoxide poisoning.
Hypoxia can occur as a result of inhalation injury, poor compliance (e.g. due to circumferential chest burns), use of opiate analgesia or sedation, or unrelated thoracic trauma.
Smoke inhalation is present in up to 30% of all flame burn presentations and occurs in higher percentages if facial burns are present. The likelihood of smoke inhalation injury is much higher when the injury occurs within an enclosed place and in cases of prolonged exposure. It is associated with high mortality and is a common cause of death at the scene of a fire.
Smoke particles settle into the distal bronchioles, causing airway damage and death of the mucosal cells. This results in an increased inflammatory response, which in turn leads to an increase in capillary leakage, resulting in increased fluid requirements and an oxygen diffusion defect. In addition, necrotic cells tend to slough and obstruct the airways. Diminished clearance of the airway also produces plugging, which results in an increased risk of pneumonia. Patients with evidence of smoke inhalation should have a baseline chest X-ray and arterial blood gas (ABG). A normal chest X-ray and ABG at presentation does not exclude inhalation injury, and these should be monitored for deterioration over time. The treatment of smoke inhalation injury is supportive.
There should be a high index of suspicion for carbon monoxide (CO) exposure in patients who were burned in enclosed areas. A diagnosis of CO poisoning can be made by directly measuring carboxyhaemoglobin levels. Patients with carboxyhaemoglobin levels of less than 20% usually have no physical symptoms. Cherry-red skin colouration is often quoted as a classical sign of CO poisoning, but in reality, it is very rare and only seen in moribund patients.
Levels higher than this can result in:
- 20-30%: headache, nausea, vomiting, dizziness
- 30-40%: confusion, disorientation, memory loss, syncope
- 40-60%: coma, hypotension, seizures, cardiac dysrhythmias
- >60%: death.
Pulse oximetry cannot be used to exclude CO poisoning as pulse oximeters are unable to distinguish oxyhaemoglobin from carboxyhaemoglobin. Pulse oximetry is often entirely normal in patients with CO poisoning, and true oxygen saturation levels should be obtained from the ABG. In addition, ABG measurements of arterial PaO2 do not reliably predict the level of CO poisoning, because a CO partial pressure of only 1 mmHg results in a carboxyhaemoglobin level of 40% or greater. Therefore, baseline carboxyhaemoglobin levels should always also be measured. The treatment of CO poisoning is via the administration of high-flow (100%) oxygen via a non-rebreathing mask initially. Once the patient has been stabilised, a specialised burns centre can be contacted for further guidance as to whether hyperbaric oxygen therapy will be of benefit.
Cyanide inhalation from the products of combustion should also be considered in patients who have suffered a burn in a confined area. The clinical features of cyanide poisoning can be similar to those of CO poisoning. A smell of bitter almonds may be present (although not everyone can detect or recognise this smell). A persistent profound metabolic acidosis is also a sign of potential cyanide poisoning. If cyanide poisoning is suspected, then a specialist poison centre should be consulted. Intravenous hydroxocobalamin (Cyanokit) is usually the treatment of choice, but some cases may require continuous venovenous hemodiafiltration (CVVHDF).
Manage circulation with burn shock resuscitation
The evaluation and management of the circulation in a patient with a major burn can be challenging. Under-resuscitation can lead to hypoperfusion and end-organ damage, while over resuscitation can worsen oedema resulting in the extension of burn depth, compartment syndrome or other complication. The ultimate goal of fluid resuscitation should be to achieve a delicate balance avoiding either of these scenarios.
In major burns, the local and systemic inflammatory response leads to capillary leak, which moves intravascular fluid into the surrounding interstitial space. This process and the resulting oedema that it causes can continue to worsen for several hours following the burn. The current ATLS guidelines recommend that all deep-partial and full-thickness burns larger than 20% total body surface area (TBSA) should receive fluid resuscitation, while some other sources suggest a lower cut off of 15%.
Intravenous access should be established with two large bore cannulas (at least 18-gauge) preferably placed through unburnt tissue. This is an opportunity to take blood for checking full blood count, urea and electrolytes, blood group, and clotting screen. If it is not possible to site the cannulae through unburned skin, an area of burned skin with an accessible vein can be used. The upper limbs are generally preferred to the lower limbs due to the increased risk of phlebitis and septic phlebitis when the saphenous veins are used for intravenous access. If peripheral veins are not available, then central venous or intraosseous access should be gained instead. Oedema resulting from the burn can dislodge the cannulae, and if the oedema is severe, the use of long peripheral catheters should be considered.
Fluid resuscitation should be with a warmed isotonic crystalloid solution, such as Hartmann’s solution or Ringer’s lactate solution. The traditionally used Parkland formula is no longer recommended for estimating fluid resuscitation, as this tended to over-estimate fluid requirements. Current consensus guidelines state that fluid resuscitation for patients with major burns should use the following formula initially:
2 mL isotonic crystalloid solution x Body Weight (kg) x %TBSA
The calculated fluid volume should then be administered as follows:
- One-half of the total fluid is provided in the first 8 hours after the burn injury
- One-half of the total fluid is administered during the subsequent 16 hours.
Children have a relatively larger surface area and smaller intravascular volume, and there should be a lower threshold for fluid resuscitation for them. Any child with a greater than 10% TBSA burn should have fluid resuscitation considered. In paediatric burns, 3 mL/kg/%TBSA should be used as the initial formula, and small children (under 30 kg) should also have maintenance fluids factored in, which should be titrated against nasogastric feeds or oral intake.
This formula should only guide the initial rate of fluid administration, and once fluid resuscitation has been commenced the amount of fluids provided should be adjusted based on a urine output target of 0.5 mL/kg/hr for adults and 1 mL/kg/hr for children weighing less than 30 kg. All patients receiving burn resuscitation fluids should have a urinary catheter inserted and have their urine output carefully monitored as a marker of perfusion.
It is important to check peripheral circulation regularly. Deep or full-thickness extremity burns can act as a tourniquet, compromising limb perfusion. If this occurs, an escharotomy may be required. An ECG should also be performed in all patients with significant burns as electrolyte and acid-base abnormalities are common and can result in cardiac dysrhythmias.
Assessing the extent of the burn
The Wallace rule of nines is a helpful way to estimate the approximate TBSA affected by a burn. It applies to areas of partial- and full-thickness burns and works by dividing the body into anatomic regions that represent multiples of 9%. In addition, the palmar surface of the patient’s hand, including the fingers, and the groin area represents approximately 1% of the patient’s body surface.
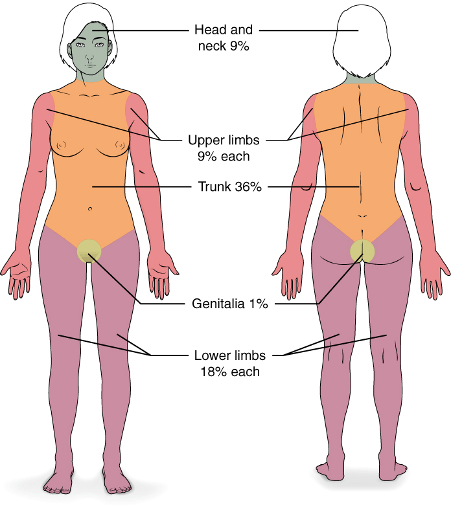
The rule of nines image sourced from Wikipedia
Courtesy of OpenStax College CC BY-SA 3.0
The distribution differs in children because of the relatively larger size of the head and smaller size of the lower extremities. The table below summarises the estimated body surface area by region in children and adults:
| Body Part | Adult BSA | Child BSA |
|---|---|---|
| Entire left arm | 9% | 9% |
| Entire right arm | 9% | 9% |
| Entire head | 9% | 18% |
| Entire chest | 9% | 9% |
| Entire abdomen | 9% | 9% |
| Entire back | 18% | 18% |
| Entire trunk | 36% | 36% |
| Entire left leg | 18% | 13.5% |
| Entire right leg | 18% | 13.5% |
| Groin | 1% | 1% |
Assessing the depth of the burn
An assessment of the depth of burn is an integral part of evaluating the overall burn severity as well as planning for ongoing wound care. Burns are usually classified as first-, second-, or third-degree, depending on how deep and severe they penetrate the skin’s surface.
First-degree burns:
First-degree burns, which are also referred to as superficial burns, affect only the epidermis, or outer layer of skin. They are characterised by erythema and pain, the skin is dry, and they do not blister. Mild sunburn is an example of a first degree. These burns do not usually require intravenous fluid replacement, are not included in the assessment of the extent of the burn and long-term tissue damage is rare.
Second-degree burns:
Second-degree burns, which are also referred to as partial-thickness burns, involve the epidermis and part of the dermis layer of skin. They can be further categorised into superficial partial-thickness or deep partial-thickness burns:
- Superficial partial-thickness burns are moist, painfully hypersensitive, potentially blistered, homogenously pink, and blanch to touch.
- Deep partial-thickness burns are drier, less painful, potentially blistered, red or mottled in appearance, and do not blanch to touch.
Third-degree burns:
Third-degree burns, which are also referred to as full-thickness burns, destroy both the epidermis and dermis and extend into the hypodermis (subcutaneous tissue). They may also damage the underlying bones, muscles, and tendons. The burn site appears translucent or waxy white or can appear charred. Once the epidermis is removed, the underlying dermis may be red initially, but it does not blanch with pressure. This dermis is also usually dry and does not weep. There is no sensation in the area since the nerve endings are destroyed.
Secondary survey and further management
Once the primary survey has been completed, and the necessary emergency management has been commenced, a secondary survey should be performed. This is a head to toe examination to look for any co-existing injuries that may have occurred.
Further management may also include the following:
- Analgesia and sedation – patients with major burns can be in significant pain or be restless and severely distressed. This should be managed with small titrated doses of an appropriate analgesic and/or sedative
- Gastric tube insertion – all patients with greater than 20% TBSA burns and those with nausea, vomiting or abdominal distention should have a gastric tube inserted.
- Escharotomies – these may be required to relieve circulatory insufficiency caused by a circumferentially burned limb
- Wound care – the burn wound should be washed, and any loose skin removed. Gently covering the burn with clean linen relieves the pain and deflects air currents. For an acute burn which will be referred to a burn centre, cling film is an ideal dressing as it protects the wound, reduces heat and evaporative losses, and does not alter the wound appearance.
- Tetanus – tetanus status should be evaluated, and vaccination may be necessary
- Antibiotics – antibiotics should be reserved for the treatment of infection only and not used prophylactically.
Header image used on licence from Shutterstock
Thank you to the joint editorial team of www.mrcemexamprep.net for this article.







Superb, excellent and Easily understand the Percentage of burn thanks