Upper limb nerve lesions are commonly tested in the basic sciences section of both undergraduate and postgraduate medical examinations and occur very frequently in the FRCEM and MRCS examinations. They are very important because they occur commonly in clinical practice but at the same time are often poorly understood by exam candidates and can be easily confused. In this series of articles we will attempt to demystify this complicated topic and deal with the most commonly occurring nerve lesions in a simple and stepwise fashion. In this first article we will start by looking at injuries affecting the brachial plexus.
Anatomy of the Brachial Plexus
The brachial plexus is a network of nerves that supplies innervation to the skin and musculature of the upper limb. It is subdivided into roots, trunks, divisions and branches and the order in which these division occur can be remembered using the mnemonic ‘Rugby Teams Drink Cold Beers’:
- Roots
- Trunks
- Divisions
- Cords
- Branches
There are typically 5 roots, 3 trunks, 6 divisions, 3 cords and 5 terminal branches as can be seen in the diagram below:
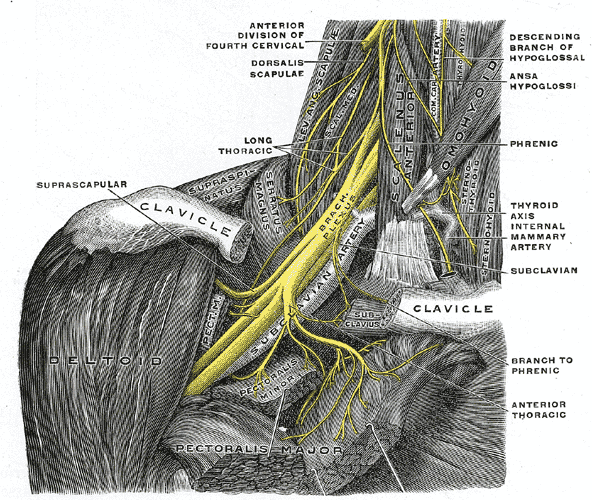
Fig 1. The roots, trunks, divisions, cords and terminal branches of the brachial plexus (from Gray’s Anatomy).
The roots
The five roots of the brachial plexus are the five anterior rami of the spinal nerves C5, C6, C7, C8 and T1. These roots pass anterior to scalenus medius and posterior to scalenus anterior before entering the base of the neck.
The trunks
The roots converge in the base of the neck to form three trunks, which are named according to their anatomical position:
- The C5 and C6 roots combine to form the superior trunk
- The C7 root continues to form the middle trunk
- The C8 and T1 roots combine to form the inferior trunk
The trunks pass laterally across the posterior triangle of the neck, where they are palpable and pass over the 1st rib posterior to the 3rd part of the subclavian artery before descending behind the clavicle.
The divisions:
Behind the middle third of the clavicle each trunk divides into two branches to form six divisions. One division passes anteriorly and one posteriorly and are therefore known as the anterior and posterior divisions:
- Anterior divisions of the upper, middle and lower trunks
- Posterior divisions of the upper, middle and lower trunks
The divisions then leave the posterior triangle of the neck and pass into the axilla.
The cords:
After entering the axilla the six divisions regroup to become the three cords. The cords lie in the axilla related to the second part of the axillary artery and are named according to their position respective to it:
- The three posterior divisions of the trunks (C5-C8, T1) reform into the posterior cord
- The anterior divisions of the upper and middle trunks (C5-C7) reform into the lateral cord
- The anterior division of the lower trunk (C8-T1) continues on as the medial cord
The branches:
The three cords give rise to five major branches in the axilla and the proximal part of the upper limb:
- Axillary nerve (C5 and C6)
- Musculocutaneous nerve (C5-C7)
- Radial nerve (C5-C8 and T1)
- Median nerve (C6-C8 and T1)
- Ulnar nerve (C8 and T1)
In addition to the fiver major branches there are several smaller branches that arise from all various parts of the brachial plexus:
| Part of brachial plexus | Branches |
|---|---|
| Roots | Dorsal scapular nerve Long thoracic nerve |
| Trunks | Suprascapular nerve Nerve to subclavius |
| Lateral cord | Lateral pectoral nerve |
| Posterior cord | Superior subscapular nerve Thoracodorsal nerve Inferior subscapular nerve |
| Medial cord | Medial pectoral nerve Medial cutaneous nerve of arm Medial cutaneous nerve of forearm |
A simple stylized version of the brachial plexus that can be easily drawn is shown below:
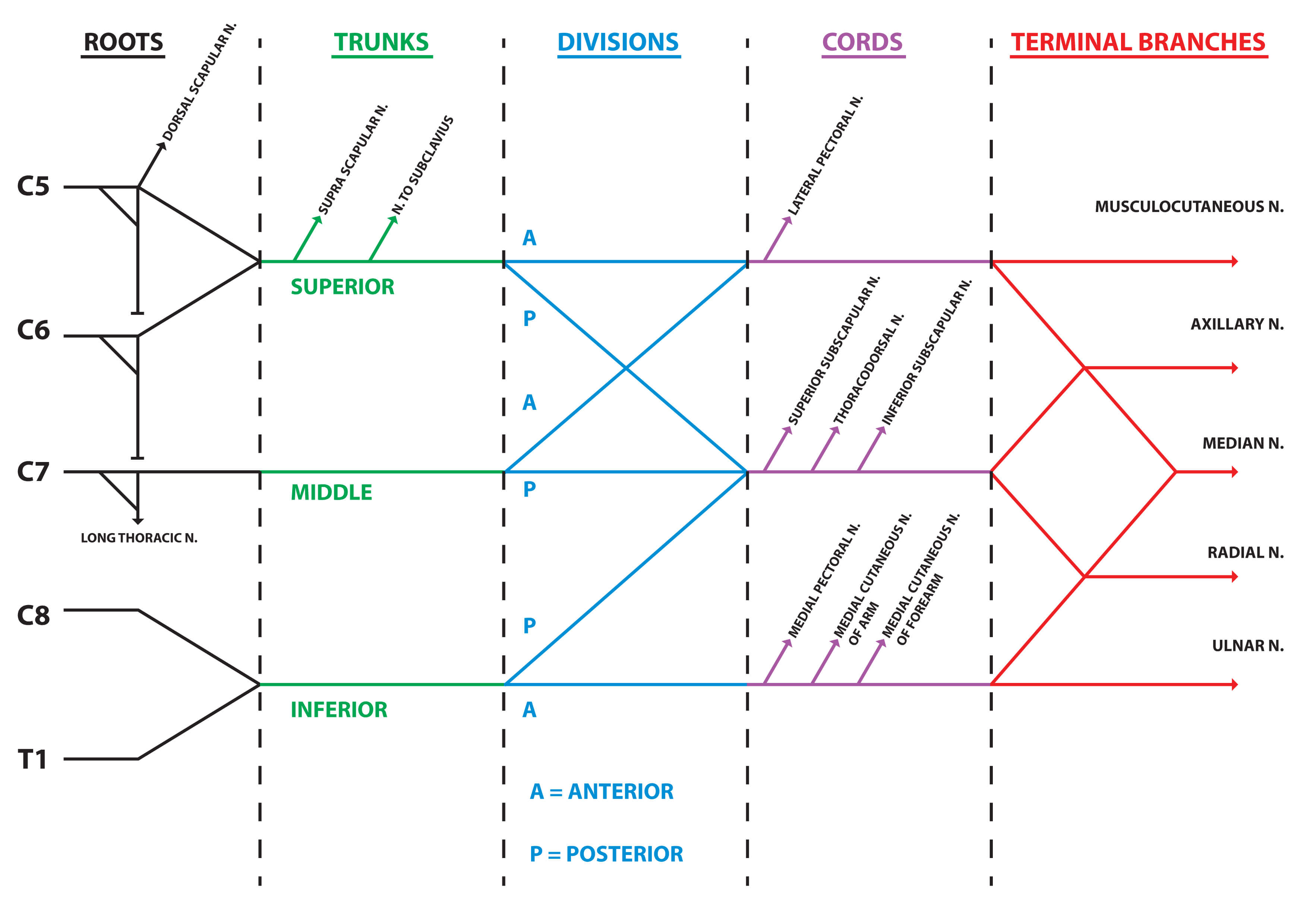
Fig2. Stylized version of the brachial plexus. © Medical Exam Prep
Upper brachial plexus lesion – Erb’s palsy
Erb’s palsy is named after Wilhelm Heinrich Erb (1840-1921), the German neurologist who described a case in 1874. The French neurologist Guillaume Duchenne (1806-1875) also described a case two years earlier in 1872 and for this reason it is sometimes referred to as the Erb-Duchenne palsy.
Erb’s palsy is a paralysis of the arm that is caused by an injury to the upper roots of the brachial plexus. The most commonly involved root is C5 but in some cases C6 is affected also.
The most common cause of Erb’s palsy is traction on the arm during difficult childbirth but it can also occur in adults secondary to shoulder trauma. Approximately 50% of cases are associated with shoulder dystocia.
Clinically the arm will hang at the side with the elbow extended and the forearm pronated (waiter’s tip sign).
On examination there will be loss of:
- Shoulder abduction (deltoid, supraspinatus)
- Shoulder external rotation (infraspinatus)
- Elbow flexion (biceps, brachialis)
Erb’s palsy can be contrasted with Klumpke’s palsy, which affects the lower roots of the brachial plexus (C8 and T1) and presents with ‘claw hand’ (paralysis of the intrinsic hand muscles) and sensory loss along the lateral side of the forearm and hand. If T1 is affected a Horner’s syndrome may also be present.
Lower brachial plexus lesion – Klumpke’s palsy
A Klumpke’s palsy, also referred to as Dejerine-Klumpke palsy, is a paralysis of the arm that is caused by an injury to the lower roots of the brachial plexus. The most commonly involved root is C8 but T1 can also be affected. The most common cause of Klumpke’s palsy is traction on the arm in an abducted position during difficult childbirth. It can also occur in adults due to apical lung carcinoma (Pancoast’s syndrome)
Clinically it presents with ‘claw hand’ deformity (paralysis of the intrinsic hand muscles) and sensory loss along the medial side of the forearm and hand. If T1 is affected a Horner’s syndrome may also be present.
Kumpke’s palsy can be contrasted with Erb’s palsy, which affects the upper roots of the brachial plexus (C5 and sometimes C6) and presents with the arm hanging at the side with the elbow extended and the forearm pronated (waiter’s tip sign). In Erb’s palsy there is loss of shoulder abduction, external rotation and elbow flexion.
Summary of Erb’s and Klumpke’s palsies:
| Erb’s palsy | Klumpke’s palsy | |
|---|---|---|
| Roots | C5/C6 | C8/T1 |
| Nerves | Musculocutaneous nerve Axillary nerve Suprascapular nerve Nerve to subclavius | Median nerve Ulnar nerve |
| Muscles | Supraspinatus Infraspinatus Deltoid Teres minor Subclavius Biceps brachii Brachialis | All small muscles of the hand (N.B. the flexor muscles in the forearm are innervated by the median and ulnar nerves but supplied by different roots) |
| Motor function | Loss of shoulder abduction and flexion, lateral rotation of the arm and elbow flexion | Paralysis of intrinsic hand muscles and ‘claw hand’ deformity |
| Sensory function | Loss of sensation along lateral side of arm | Loss of sensation along medial side of forearm and hand |
Next: Upper Limb Nerve Lesions Part 2 – The Radial Nerve
Thank you to the joint editorial team of www.anatomyprep.co.uk for this ‘Exam Tips’ blog post.
Header image used on licence from Shutterstock





I like it.. Very good.
Thanks! very good lesson
good
I am very happy …for this lesson
I think very good lession