In Part 2 of our ‘Upper Limb Nerve Lesions’ series we learnt about the radial nerve and the most commonly occurring lesions associated with damage to it. We now move on to the median nerve and it’s associated nerve lesions.
The median nerve is a major branch of the brachial plexus that is derived from the medial and lateral cords. It contains nerve fibres from all 5 roots of the brachial plexus (C5 – T1). It supplies the flexor muscles in the anterior compartment of the forearm (apart from flexor carpi ulnaris and part of flexor digitorum profundus, which are innervated by the ulnar nerve), the thenar muscles and the lateral two lumbricals. It supplies sensory innervation to the lateral side of the palm and the lateral three and a half fingers on the palmar surface of the hand.
Anatomy of the Median Nerve
The median nerve arises in the brachial plexus and enters the arm from the axilla at the inferior margin of teres major. It initially lies anterior to the axillary artery and then lateral to it and then descends down the arm lateral to the brachial artery. It then crosses over the brachial artery at the level of the mid-humerus to lie medial to the artery in the cubital fossa.
The median nerve passes beneath the bicipital aponeurosis at the elbow and leaves to cubital fossa between the two heads of pronator teres to enter the anterior compartment of the forearm. Here it crosses superficial to the ulnar artery and gives off its anterior interosseous branch below this
It then travels between flexor digitorum superficialis and flexor digitorum profundus before emerging between flexor digitorum superficialis and flexor pollicis longus about 5 cm proximal to the wrist. Here it gives off its palmar cutaneous branch and then passes deep to flexor retinaculum between the tendons of flexor digitorum superficialis and flexor carpi radialis. Once in the hand it gives off its terminal branches: the recurrent (muscular) branch and the palmar digital branches.
Fig 1. The nerves of the upper left extremity, showing the course of the median nerve (from Gray’s Anatomy).
The Motor Function of the Median Nerve
The muscles supplied by the median nerve and its motor branches are shown in the table below:
| Branch | Muscles supplied |
|---|---|
| The median nerve | Pronator teres Flexor carpi radialis Palmaris longus Flexor digitorum superficialis |
| The anterior interosseous nerve | Flexor digitorum profundus (lateral ½) Flexor pollicis longus Pronator quadratus |
| The recurrent branch | Thenar muscles - Opponens pollicis - Abductor pollicis brevis - Flexor pollicis brevis |
| The palmar digital branch | 1st and 2nd lumbricals |
The Sensory Function of the Median Nerve
The sensory function of the median nerve is provided by its two main sensory branches:
- Palmar cutaneous branch – supplies the lateral aspect of the palm (arises in forearm and does not pass through carpal tunnel)
- Palmar digital branch – supplies the palmer surface and fingertips of lateral 3 ½ digits (arises in hand)
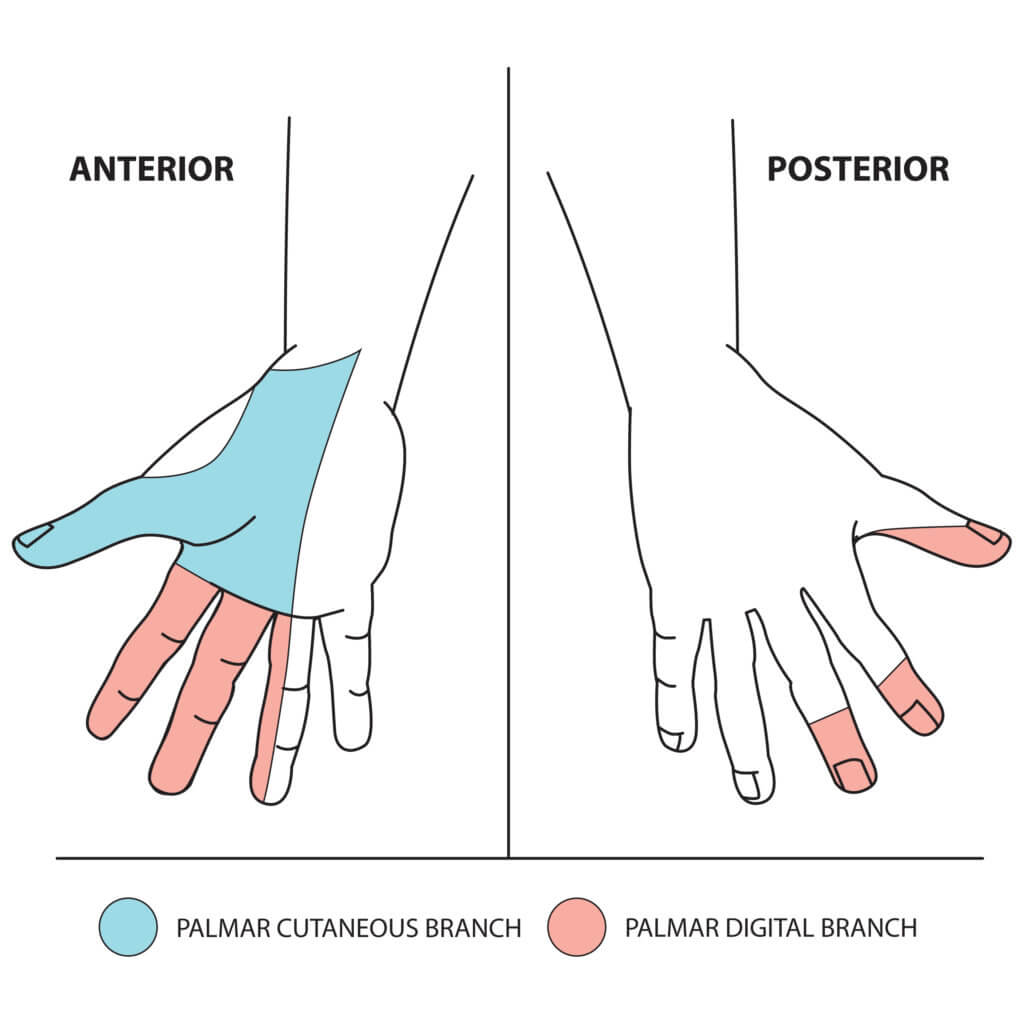
Fig 2. The sensory function of the median nerve. © Medical Exam Prep
Median Nerve Lesions at the Elbow
The median nerve can be damaged by injury to or at the elbow. The commonest mechanism of injury is supracondylar fracture of the humerus.
Motor damage:
All of the flexors and pronators of the forearm will be paralysed (apart from flexor carpi ulnaris and the medial ½ of flexor digitorum profundus, which are supplied by the ulnar nerve), which will result in weakness of wrist flexion and abduction. There will also be loss of thumb abduction and opposition due to loss of the muscles innervated by the recurrent branch. The 1st and 2nd lumbricals will also be paralysed and the patient will be unable to flex at the metacarpophalangeal joints of the index and middle fingers. The characteristic papal benediction sign will be evident, there will be prominent thenar wasting and there will be ulnar deviation of the wrist
Sensory damage:
There will be loss of sensation over all cutaneous areas innervated by the median nerve.
Papal benediction of the hand:
Papal benediction occurs due to median nerve damage at the elbow. In contrast to the ‘ulnar claw’ it is only apparent if the patient is asked to make a fist.
When asked to make a fist, the patient will be able to flex the little and ring fingers, which is performed by the medial half of flexor digitorum profundus and the ulnar two lumbricals (innervated by ulnar nerve). The patient will not, however, be able to flex the index and middle fingers due to loss of the anterior interosseous nerve.
Therefore, when the patient attempts to make a fist, a claw shape will occur, where the little and ring fingers are flexed and the index and middle fingers are extended:

Fig 3. Papal benediction of the hand.
Median Nerve Lesions at the Wrist
The median nerve can be damaged by injury at the wrist by lacerations proximal to the flexor retinaculum. The nerve can also be compressed in the carpal tunnel.
Motor damage:
There will also be loss of thumb abduction and opposition due to loss of the muscles innervated by the recurrent branch. The 1st and 2nd lumbricals will also be paralysed and the patient will be unable to flex at the metacarpophalangeal joints of the index and middle fingers. Wrist and finger flexion will be intact as the anterior interosseous nerve is unaffected. There will be thenar wasting but no ulnar deviation of the wrist or papal benediction.
Sensory damage:
There will be loss of sensation over the lateral 3 and ½ fingers and nail beds and the lateral side of palm. It should be noted that the lateral side of the palm can be preserved as the palmar cutaneous branch can be spared.
A comparison of median nerve lesions at wrist and elbow is shown in the table below:
| Median nerve at elbow | Median nerve at wrist | |
|---|---|---|
| Motor loss | Weak wrist flexion and abduction Loss of thumb abduction and opposition Loss of flexion of index and middle fingers | Loss of thumb abduction and opposition Wrist and finger flexion intact (due to intact AIN) |
| Sensory loss | Lateral 3 and ½ fingers and nail beds Lateral side of palm | Lateral 3 and ½ fingers and nail beds Lateral side of palm (but can be preserved depending upon palmar cutaneous branch) |
| Hand deformity | Ulnar deviation of wrist Thenar wasting Papal benediction on flexing fingers | Thenar wasting No ulnar deviation of wrist or papal benediction (due to intact AIN) |
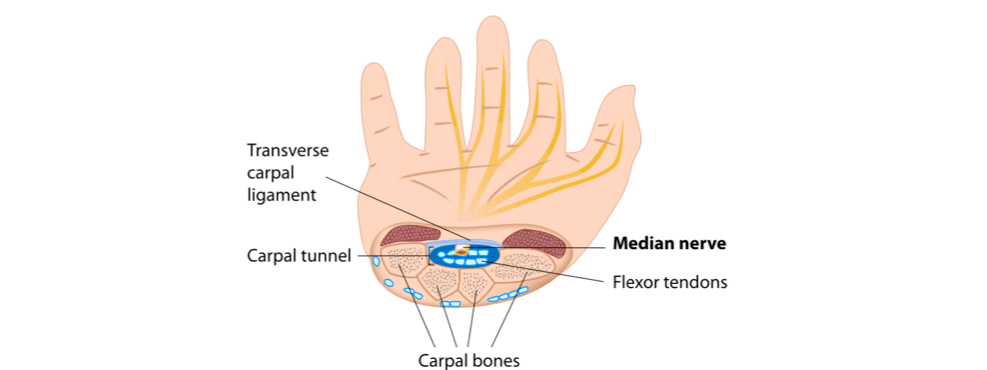
Carpal Tunnel Syndrome
Carpal tunnel syndrome is due to compression of the median nerve as it passes under the flexor retinaculum. This causes parasthesia and pain in the lateral 3 and a half digits and wasting of the thenar eminence. The symptoms are often worse at night.
Most cases of carpal tunnel syndrome are idiopathic, but risk factors include:
- Obesity
- Oral contraceptive
- Hypothyroidism
- Rheumatoid arthritis
- Pregnancy
- Diabetes
- Amyloidosis
- Acromegaly
- Tumours compressing on the carpal tunnel
- Previous fractures of the wrist
Tinel’s test involves tapping over the carpal tunnel. It is positive if this produces parasthesia. Phalen’s test involves hyperflexing the wrist for a minute. Again this is positive if it reproduces the symptoms of carpal tunnel syndrome. If the diagnosis is uncertain, nerve conduction studies can be requested. Treatment of carpal tunnel syndrome involves the use of a night splint that holds the wrist in dorsiflexion. More severe cases can be treated using corticosteroid injection or surgical decompression.
Next: Upper Limb Nerve Lesions Part 4 – The Ulnar Nerve
Thank you to the joint editorial team of www.anatomyprep.co.uk for this ‘Exam Tips’ blog post.
Header image used on licence from Shutterstock





Nice